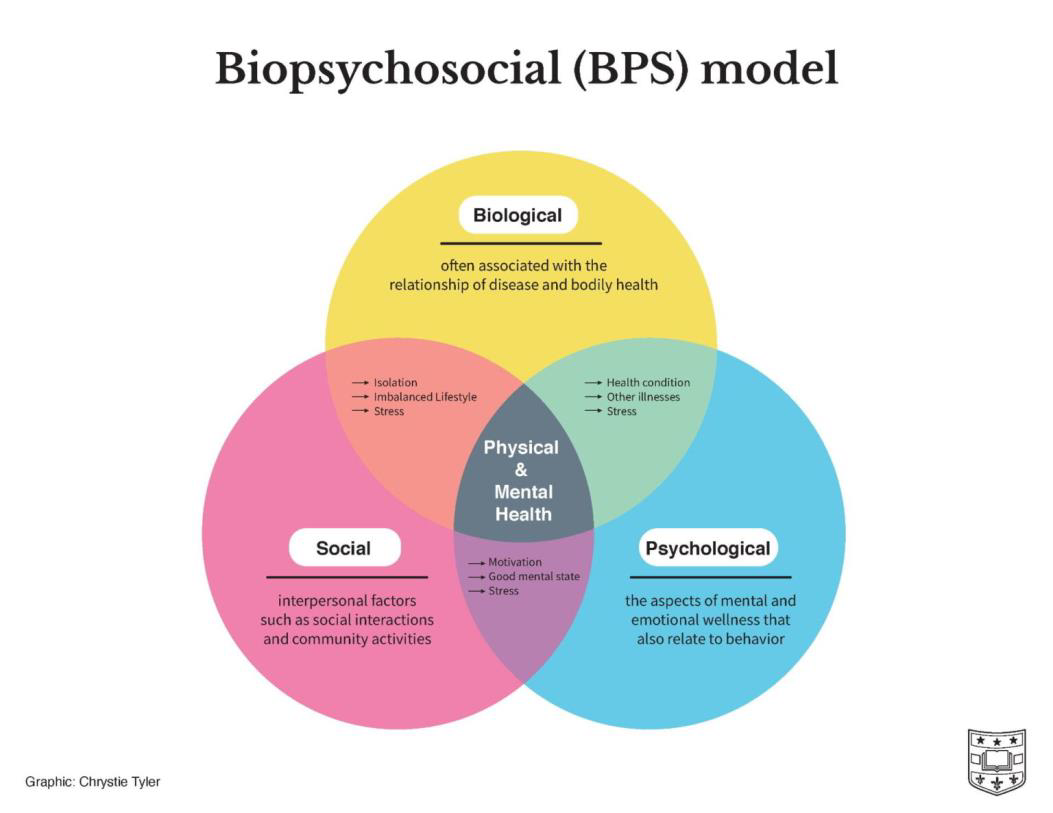
The biopsychosocial approach involves three key systems that affect a person’s recovery: biological, psychological, and social. This model, also known as the biopsychosocial model, helps care providers look beyond just the diagnosis to create more comprehensive treatment plans. By understanding how these systems overlap and interact, care plans can be customized to meet each patient’s specific needs.
Health care providers often can’t be physically present for all patient care and recovery programs. Fortunately, advancements in HealthTech are bridging the gap between home and clinic care, with our Recovery+ program being a prime example. Recovery+ is a health coaching platform that uses a psychosocial framework to speed up recovery and improve the return-to-work process for injured workers. Although learning about the biopsychosocial framework and its role in employee recovery might seem overwhelming at first, it is quite beneficial.
The three systems of the biopsychosocial model are:
- Biological : Factors like pain and movement disorders.
- Psychological : Elements such as avoidance behaviors and anxiety.
- Social : Issues like financial worries and isolation.
The Recovery+ program uses Patient Reported Outcomes (PRO) assessments to gather feedback on patients’ emotional and physical states. This data helps coaches identify relevant activities and provides therapists with crucial insights to ensure recovery milestones are achieved.
The 5 P’s of the biopsychosocial model, while not originally part of it, offer a way to further categorize the three systems (biological, psychological, and social) to help clinicians and researchers consider various factors affecting health and well-being. These categories help in addressing patient needs more effectively.
- Presentation of the Problem : This refers to the main health issue or condition a person is struggling with, which could be a physical illness, mental health concern, or social challenge.
- Predisposing Factors : These are characteristics that make a person more susceptible to certain diseases, including genetic predispositions, early life experiences, and personality traits.
- Precipitating Factors : These are events or conditions that trigger the onset of a health condition or worsen existing symptoms, such as life stressors, traumatic events, or changes in health status.
- Perpetuating Factors : These factors maintain or prolong a health condition once it has developed, often categorized as psychological or social. Examples include persistent stressors, maladaptive coping mechanisms, and environmental factors.
- Protective Factors : These factors enhance resilience and improve health, such as social support, positive coping skills, and access to resources.
The biopsychosocial model offers a more holistic understanding of health and illness compared to the traditional biomedical model, which only considers biological factors. It fosters interdisciplinary collaboration, supports preventive care, and enhances overall well-being.
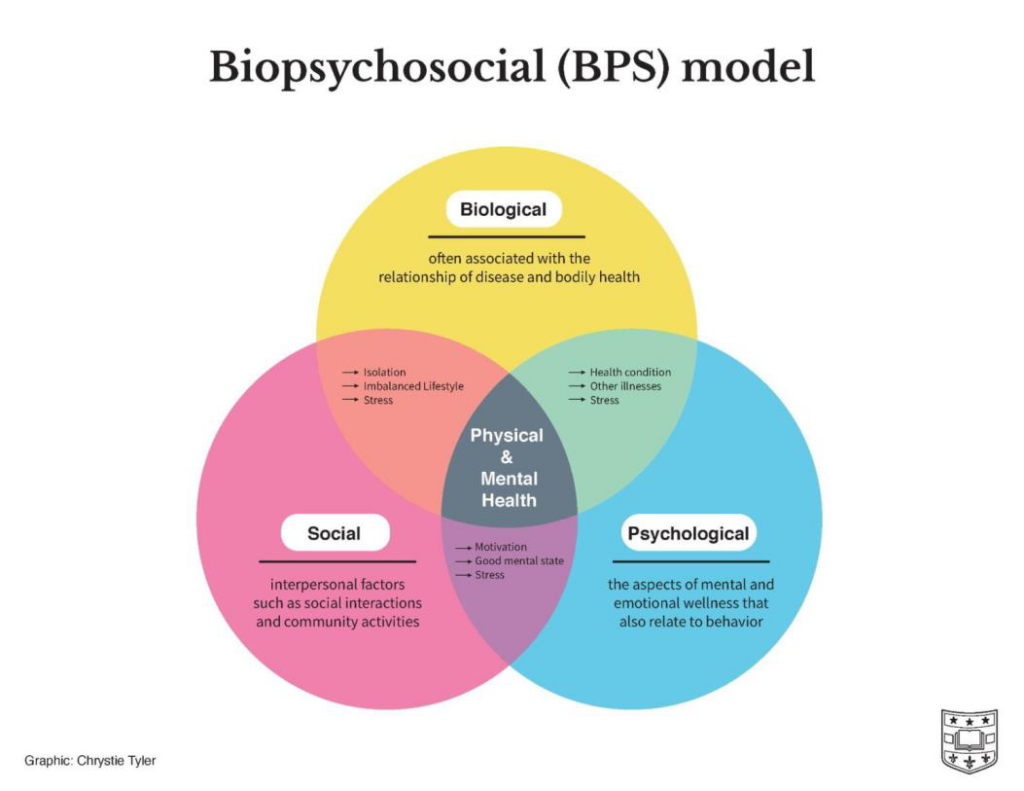
Biopsychosocial Model: an Overlapping system
Biological Factors
- General medical history
- Substances & medications
- Genetic predisposition (family history)
- Disturbances of the biochemical, neuroendocrine, or immune systems
Psychological Factors
- Psychodynamic factors; childhood experiences
- Childhood abuse history
- Psychological traumas
- Temperament
- Personality disorders
Social Factors
- Employment
- Finances
- Relationships
- Housing
- Legal issues
- Religion
- Culture
- Education
The Biopsychosocial Approach to Treat Depression
Biological models view depression as a consequence of genetic vulnerability or biological disturbances of the biochemical, neuroendocrine, or immune systems.
Psychological models highlight the importance of cognitive and behavioral schemas. These schemas reflect the individual’s fundamental views and may represent earlier experiences in life that dominate information processing at the present time.
Sociocultural risk factors include changes and instability of many societal aspects that may have an impact on the vulnerability of the individual.
Biological
- Treating and stabilizing underlying medical problems.
- Treating substance abuse disorders with goal of achieving sobriety.
- Treating primary psychiatric symptoms with known biological treatments including: psychotropic medications, electroconvulsive therapy (ECT) and repetitive transcranial magnetic stimulation (rTMS).
Psychological
- Psychotherapy modalities including but not limited to: Cognitive-Behavioral, Psychodynamic, Supportive, Dialectical Behavioral, etc.
Social Interventions
- Initiating referrals
- Assessing support systems
- Advocating for your patients
- Accessing community resources
- Funding
- Insurance coverage
- Case managers
- Social workers